Prognostic Indicators
"What’s your prognosis?”
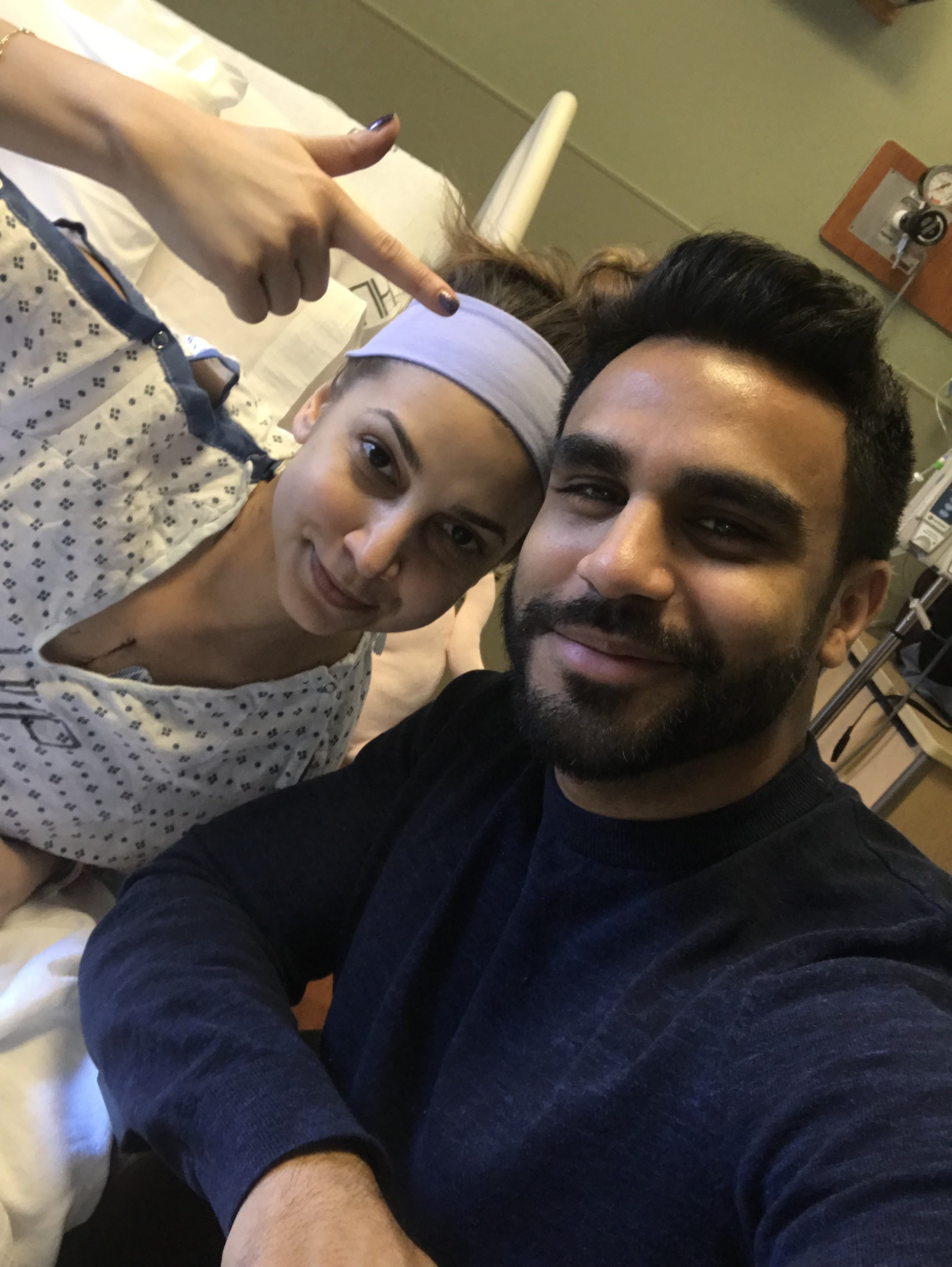
I get asked this all of the time. When did this become socially acceptable? Lucky for you, I’m an open book with a loud mouth. I'm inquisitive. And I have been trained to think scientifically.
I can go through many different percentages for you. According to a paper published by Dr. Anyanwu in 2003, 20% of heart recipients die within a year of the transplant operation. Afterwards, the death rate is 4% per year for the next 18 years, so that 50% of patients can expect to be alive after 10 years and 15% after 20 years.
Or I can take a stroll through downtown Philly (with my Nikon in hand), while taking photographs of the skyscrapers that overlook the city that I’ve called home for the last three years. During this stroll, there is a small chance that I will get hit by a car. According to national statistics, there is a 1 in 572 chance that I will die after getting hit by that particular car. It will likely be from blunt force trauma. I will hemorrhage internally, and die a fast or slow death (depending on which organ has been lacerated).
I can carefully search the internet for the descriptive statistics regarding heart transplants— the medians, the maximums, the minimums, the averages of life expectancy. I can educate myself about our mortality rates. My own mortality rate. According to UpToDate, the median survival for heart transplants between 1982 and 2015 was 11 years for adult recipients. Many adult patients die about a decade after transplant. Younger patients usually live longer than that. I can anxiously look up the definition of “young” in two separate peer-reviewed articles.
Or I can take the time to tackle my next feat. I have always wanted to get my pilot’s license. I was going to do it at some point after my medical training was complete. So, I can sign up for a course and start flying through the horizon, checking off another one of my life’s ambitions. But did you know that there is a chance that I will die while conquering this goal? According to Statistica, 561 people died in air crashes around the world last year. So my plane may crash from some sort of incorrect measurement, perhaps the plane’s fuel will be miscalculated. Most likely (55% of the time), it will be from pilot error— my own ignorance. I will die from penetrating trauma or pressure-related injuries, and my body will burn, slowly, into charred nothingness.
I can rummage through my desk and find my ripped-up medical textbooks. Or my old notes and Powerpoint presentations from medical school. I can look through the high yield facts that we quickly glanced over about heart transplant patients and their medical histories, the few scribbles I had written down about their terrifying complications. I can remind myself that many heart transplant patients die a slow, painful death after being diagnosed with metastatic cancer. Usually by lymphoma, squamous cell carcinoma, or basal cell carcinoma.
Or I can take the next train to New York City. Or Baltimore. Wherever I feel like going. I can drag someone with me, or I can go alone. But this comes with a potentially fatal risk. According to the US Department of Transportation, there are about 5,800 train-car crashes each year in the US. These cause 600 deaths and injure about 2,300 people in total. So, there is a chance that I will die on the train after an awful collision with a car that just didn’t see us coming. It will be an instantaneous death, after a handrail gets jammed into my chest causing a bleeding gash right through my heart. My cardiovascular system will come to a sudden stop. And then I will die.
I can ask my doctor about my future co-morbidities. Academic discussions, or as I like to call them, “doctors doctoring doctors." By the sixth year after transplantation, most heart transplant patients will have hyperlipidemia, or high cholesterol levels. About a third will have a rise in their creatinine levels, aka failing kidneys. A third will suffer from coronary artery disease. A fifth will have experienced some sort of cancer.
Or I can call my parents. I can talk to them to pass the minutes this evening, because I just can’t seem to fall asleep. I can listen to their voices telling me to make sure that I eat, make sure that I stay warm. There is a chance that an unknown someone will then barge into my apartment. I will tell my parents to hold on, and I will open my bedroom door to find a person burglarizing my home. That person will then kill me, most likely with a gun. A gun shot wound to the head, or maybe (more likely) a gunshot wound to the chest. According to 2014 national databases, there are 15.9/100,000 random homicides yearly in Philadelphia, one of the most dangerous cities in America. So I will become a fatal statistic. Random home invasion, random homicide. Cause of death: (most likely) gunshot wound to the chest.
I can Google the longest someone has lived with a heart transplant for. 33 years. That can’t be right. I can Google it again. 33 years????? Perturbed, I can then think about how I won’t even make it to 65. Holy s&%#.
Or I can listen to Tribe’s Beats, Rhymes, and Life in my apartment (on volume 11). I can decide to invite a few people over for a game of Cards Against Humanity. Maybe I can have a beer with them, too. But, damnit— alcohol intoxication can also kill. According to the CDC, about 6 people die of alcohol intoxication every day in the US. So there is a chance that I will die from one too many beers that interacted poorly with my transplant medications. And it won’t be pretty, either. Altered mental status, hypothermia, respiratory depression, cardiac arrest, death.
I can look up the fancy prognostic indicators— the things that put me at risk for early death. They say that prognosis depends on things like ischemia time of the heart (174 minutes). It also depends on how old you were at the age that you were transplanted (30 years, 49 weeks old) and how young the donor was at the time of death (unsure).
Or I can go for a jog, feeling the early spring wind against my face. Feeling every muscle in my body slowly get stronger after months of being deconditioned— I can take the pain. My determination and my willpower speak for themselves during these moments. However, there is a chance that I will suddenly die during this invincible jog. In medicine, we call it sudden cardiac death. I will begin experiencing an arrhythmia that my transplanted heart was statistically more prone to than a healthy native heart was. I will clench my chest, fall over, and die. Someone will find me in a few minutes. They will try to save me. But, according to national prehospital data, I will likely be dead upon arrival to the emergency department.
I can spend hours upon hours meticulously punching in the numbers, searching the resources in our medical libraries, asking the cardiologists and the epidemiologists— what exactly is my prognosis?
Or I can take the time to breathe. To live. To laugh. To cry. To love.
To write my thoughts out and think about the beauty of life, the irony and the mystery of this thing that I’ve been given (twice actually, technically).
To smile.
To be grateful. To be happy. To be angry.
To feel.
To remember that, for all of us-- not just for me-- life is finite.
The scientific values and prognostic indicators and the medians and means and the what-if's and why-not's don’t change this one thing that we all have to remind ourselves (unfortunately) more often than we should:
that, ultimately,
life
is
finite.
Until next time, from William Saroyan’s The Time of Your Life:
“In the time of your life, live—so that in that good time there shall be no ugliness or death for yourself or for any life your life touches. Seek goodness everywhere, and when it is found, bring it out of its hiding place and let it be free and unashamed.
Place in matter and in flesh the least of the values, for these are the things that hold death and must pass away. Discover in all things that which shines and is beyond corruption. Encourage virtue in whatever heart it may have been driven into secrecy and sorrow by the shame and terror of the world. Ignore the obvious, for it is unworthy of the clear eye and the kindly heart.
Be the inferior of no man, or of any men be superior. Remember that every man is a variation of yourself. No man's guilt is not yours, nor is any man's innocence a thing apart. Despise evil and ungodliness, but not men of ungodliness or evil. These, understand. Have no shame in being kindly and gentle but if the time comes in the time of your life to kill, kill and have no regret.
In the time of your life, live—so that in that wondrous time you shall not add to the misery and sorrow of the world, but shall smile to the infinite delight and mystery of it.”