It was inevitable— Hahnemann University Hospital was going to close, and so was our Emergency Medicine program.
A bit of history about our program. It was one of the first EM programs ever. It was founded in the early 1970s, when Emergency Medicine was just a new field. Dr. Dave Wagner. Dr. Jim Roberts. We had a running list of all of the great names that started the program and trained in the program. It had hundreds of alumni around the nation.
And just like that, it was going to close.
And here I was. Fresh out of heart transplant surgery. Just about to show the world that I could do it again. With no place to do it at.
So, we were told to start looking for new residency programs. We were going to be residency-less. In the medical world, this = “orphaned” residents.
By the way, right around this time, I felt like DeMarcus Cousins after his Achilles’ tendon rupture. I was Alin, right after my heart transplant. Hahnemann was my original team; they knew me. But I was a free agent now. The other teams (residency programs) knew that I was probably good, and respected everything that I had been through, but could they have taken a chance on me? My heart was my Achilles’ tendon, my fate was in the hands of the NBA draft— uh, ReMatch 2019.
I was DeMarcus Cousins.
And I had to think positively.
I kept telling myself: I had already matched into a wonderful Critical Care Medicine fellowship program— one of the toughest, best in the nation (and that was the most ironic part of my whole story … that I had matched into an ICU fellowship just weeks before becoming an ICU patient, remember?). I was projected to start July 2020. So all I needed was a place to complete my last few months of residency. My procedures had been signed off. Almost everything had been done. I just had to finish my shifts, take my boards. Move to New York City. And get on with this shit. I had to move forward.
Furthermore, I had to stay in the Greater Philadelphia area to complete my residency— it would be ideal if I could continue my heart transplant care at UPenn (for at least this first year).
Luckily, there were many three-year EM residency programs in the area-- this was going to be easy. I had great evaluations, tons of research, I was literally almost done w residency, and I obviously had some sort of decent application— I had gotten into fellowship with the same application. If anything, I had added a few more things to my CV since my heart transplant.
This was going to be easy. Easy peasy.
I interviewed at a few Philly-based EM programs. In total, there were over 500 residents who were going to need spots in various specialties and most of them wanted to stay in Philadelphia. From these 500+ residents, 46 of us were specializing in Emergency Medicine.
Anyways, interviews came and went. And I waited and waited for some sort of offer from any of the seven nearby programs. ONE would surely take me. A few of them seemed pretty excited to have me as a potential resident.
And so I waited for an offer.
And waited.
And...
No.
No offer.
Of course.
So there was my third battle of the summer. I became one of the few residents who did not find an easy residency spot in the city. And I legitimately needed a spot in the city. Like, legit, legitimately.
I wasn’t very open about my third battle. I was ashamed of my third battle. I was so upset by it that I remember I stayed in bed for 24 hours on that Thursday, something that I never, ever do. I didn’t say a word to anyone. I took a Benadryl by 9pm that night, and just went back to sleep in the bed that I had laid in the whole day.
Because there was no f&%$ing way that not one thing couldn’t go right for me this year.
I was so sad that I couldn’t even be angry or sarcastic about what had just happened. I was so sad that I couldn’t even call my friends or my parents.
I didn’t find a residency spot in Philadelphia. What did this mean for me?
I was told that these programs would automatically take me because of my situation and my need to stay in the city. I trusted the people around me. I didn’t transfer my heart care to any new hospital system. This will take weeks to do if I have to move.
If the program closes tomorrow, I have no program to get transferred to. Thus, no health insurance. Will I have health insurance benefits for the next few weeks while I search, since my employer is filing for bankruptcy?
I just got off of medical leave. No more COBRA for me. Can I go back on COBRA?
If I have no health insurance, how will I pay for my expensive medications this month? I think Tacrolimus costs thousands of dollars.
When is my next Tac refill?
Do I need to reschedule my Cath?
What if I don’t find a residency in time and just never finish residency?
What if I just never find a job ever again? Should I have been more private about my transplant?
Is this the third sign just honestly telling me to give up on everything?
You know, I even remember thinking the darkest thought of all:
that this would have been so much easier if I had just died in December.
Because dying in those few seconds during that winter evening, when everything in my head was really peaceful and calm (I still remember just those last seconds vividly "should we just turn it into a code")— that would have been much easier on my heart than having to go through sudden transplant surgery. Months of quarantine, anxiety, setbacks. An episode of acute rejection. Biweekly cardiac catheterizations. Weekly lab draws. A residency program closure. Anger. A rising creatinine level. Loneliness. Stress. Unemployment. Worry.
Constantly hoping for the best, expecting the worst, and then just being handed the worst.
Was this my breaking point?
People kept asking me how I hadn’t reached my breaking point yet. “If I were you, I would’ve killed myself by now!” (which is also a terrible thing to say to someone, by the way)
Well, you aren’t me. And if by all that you mean, “How the hell are you handling all of this?” I didn’t choose for any of this to happen to me. So it hurts me when you say that. I am trying my best, and I don’t want to kill myself, and maybe you shouldn’t say that to me. It doesn’t make me feel stronger. It just makes me feel like my life is not worth living. And to say that to someone who’s been given a second chance to live … you just wouldn’t know how that feels.
And I just wish one f&^%ing place would’ve taken me here in Philadelphia.
Ugh.
I fell asleep with the most negative thoughts in my head. I felt some palpitations. I had a migraine headache. I don’t think I even ate that day. And I didn’t even care.
I woke up on Friday morning, still a bit sad. Groggy from the Benadryl. I took my morning medications, looked through my emails to make sure that no program truly wanted to make an offer for this poor transplanted PGY3 who was almost done with residency (nope).
I wasn’t as sad that day; I was just bitter. Angry. Ready to figure out why I hadn’t gotten an offer.
But then I found out that a lot of my third-year co-residents also hadn’t gotten offers. Many of them were struggling for their own reasons. One of them had just had a baby, had just bought a house in the area. One of them had already transferred residencies one other time— his previous residency program had also closed (his luck was just as bad as mine, we had decided). Actually, a lot of us had had really sad Thursday nights. Our attendings called us, talked to us. Our co-residents sent us positive messages. Friends and family told us that everything would be okay. (Worst thing to say, btw, just don’t ever say that to anyone.)
Everybody wanted to help. The only problem was that, well, nobody knew how to help.
We didn’t even know how to help ourselves.
We went out for some food, beers. We cried. We hugged. We were all so helpless, even those who had found residency spots.
“It’s not gonna be the same. I’m gonna be alone with random people. And we’ve always been the misfits around here,” one of the residents said.
“I just feel weird because everyone keeps saying that they want to help us and I just want to be, like, all right then get me into your freakin’ program and make it into Drexel EM and we’ll be good,” I said.
And don’t forget. These people weren’t just my co-residents. They were something else for me. My life had been saved at Hahnemann. I had died in one of those rooms, and it was the Drexel EM, IM, Surgery residents and nurses who saved my life that first time. My first ever central line had been placed by the Drexel Pulm/Crit fellow. The Drexel Cardiology team had first taken me to the cath lab.
Nobody would ever understand the emotions that I felt during the summer of 2019.
And some of us still needed to find a hospital to finish our training at.
We could hate that CEO who decided to shut down Hahnemann all we wanted. But the system let this happen. I couldn’t blame him for my migraine and my palpitations. My co-resident couldn’t blame him for now having to sell his house in Philadelphia to move elsewhere. And that was just us. Remember, this closure affected our patients, too. Where would they get their care? And now, the nearby hospitals were going to become more saturated— longer ED waiting times, worse outcomes for hospitalized people. This whole thing was a complete catastrophe for all of us.
Anyways … why didn’t I get an offer in Philadelphia?
I knew that funding would have been an issue with me (a resident with just a few months of residency left … this is too complicated to explain, but trust me on it), and that I was “off-cycle” (aka a “headache” with paperwork, boards, everything in between for a program director). Maybe my scores sucked. Maybe my evals sucked. Again, I have no idea. If I had gotten into a fellowship program with that application, then no, I don’t think so, but who knows.
And was my health an issue? Who knows. Probably. But what was I supposed to do? Delete my blog and hope that nobody remembered me ever again? I was a bit unforgettable at that point, I assumed. And I was glad. Good. Unforgettable and proud. If I was going to be unemployed for the rest of my life, then at least I had made a difference in the world of organ donation. So be it. Bye, Felicia.
I called my Transplant Team. And, of course, I was overly dramatic as usual. “So basically I’m unemployed AND immunocompromised and I am so upset by this whole thing and UGH…”
It was true. I had no job. I had no immune system. I probably had no health insurance.
My social worker helped me out a lot. We were able to get me extra prescriptions in case I ran into insurance issues. People were worried about not re-matching into their top choice residency programs and here I was worried about, like, making sure that I would be able to stay alive another month. Which I thought was hilarious. Good, my dark humor was coming back.
She offered to call the ACGME, even nearby programs, to see if we could get something figured out. I had some special (critical) circumstances related to my health, surely something could or would happen? I told her not to get her hopes up.
Over the next day, my sadness turned into anger. Turned into rage. Turned into pure energy to figure this shit out asap.
“Resilient” was my middle name. (See my first post that I wrote on post-op day 7. S/p heart transplant surgery.) Ha. This was just another Inconvenient Life Event to add to my year. And I was going to embrace it.
I wish I could tell you that the most magical and craziest thing happened that miraculously placed me into a nearby residency program.
But what actually happened was that during that weekend, I just decided to Google the words: “residencies near Philadelphia.” And I just decided that I would email every single residency program director around the area.
Was this cold calling? Unprofessional? Walk a mile in my shoes— you would’ve done the same.
I got around to emailing one, something along the lines of:
“Hi. My name is Alin. I need a spot for last few months of residency. I have a heart transplant (done at UPenn), must stay in area. You might know me. But I had goals before the transplant as well. Already have fellowship for July. I have a beautiful CV (attached). Kthxbye.”
I spoke to the program director the following day. As it turned out, he did know about me. As it turned out, he was starting up a new program and was very open to taking a few of the Hahnemann residents. Because of my interest (uh, Google search & desperate email), some of us actually ended up interviewing there.
The next day, he called me and asked, “So this is me formally asking you, if you’d like to join our program?”
And I remember telling him, “AHHHH this is the best phone call, well, second best phone call of this year! You saved my life! You’re right up there with the phone call I got about my heart!!!!!!! I’m so in! I’m in! This was like LITERALLY the worst week of my life, well like the second worst week of my life next to that one time when my heart stopped….”
And he was just laughing on the other line. And I was laughing. And just like that, in the strangest way, it worked out. I was in the lobby of my apartment building, and everything felt okay again.
He even made me Chief Resident, coming up with a plan on how I could do part-time admin/clinical duties simultaneously, as that would be much less stressful for me (and my health) at this time.
He was more than flexible with my health needs. “Sorry, I get labs drawn like all of the time, but I won’t miss any conference days for them.” That was no problem for him.
The whole program, including the other faculty and residents, were very welcoming.
So I ended up at UPMC Pinnacle with my co-resident. (A train ride away, but close enough. I mean, what can I do?) … I’ve been there for a little over a month now, and everything has been going well so far. Plus, I have funny stories to share about what it’s like using public transportation again as a transplant patient.
Also, I got to keep my Transplant Team at UPenn. And I love them to death because they saw how much more stressed I was about the Hahnemann debacle than I ever was about my heart transplant, and they were by my side the whole time.
A lot of people (other than friends/fam) were by my side— from the Drexel faculty, the Hahnemann staff, and mostly all of my Twitter friends. <3 I appreciated that.
And I love chaos and I love the unknown and I love craziness. I am the definition of an adrenaline junkie. “Come at me bro” with everything.
But I just really hope the next few months are stable and normal for me.
No more sudden catastrophes, please.
To end this, here are some things that you may be interested in:
1) NEJM’s Dr. Lisa Rosenbaum interviewed me and a few others about the effect of Hahnemann’s closure - read it here.
2) I wrote this piece in JACC for all of you who work in healthcare. You work hard. Please read it. I mean every word. Thank you for all that you do.
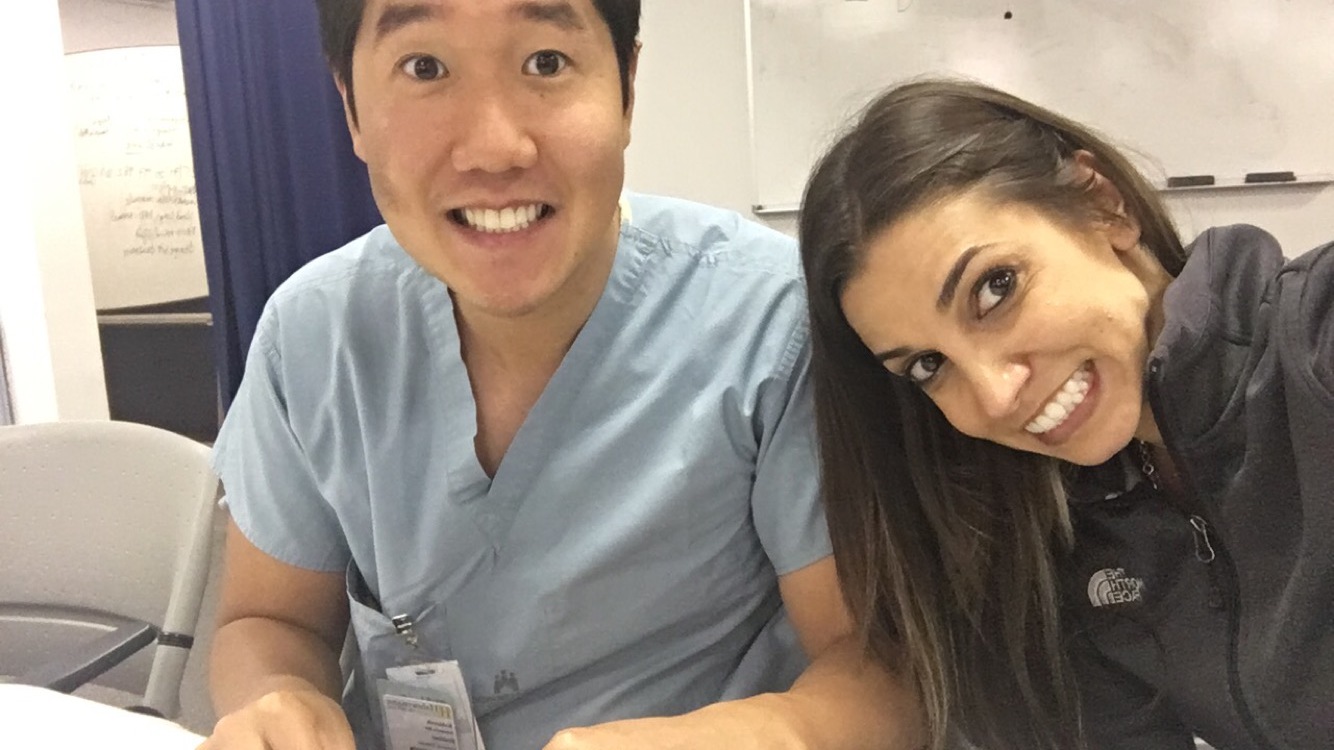
3) Pics from Summer 2019 (between Philly & the H-Burg)